Radiotherapy
Radiation therapy uses high-energy radiation to shrink tumors and kill cancer cells. X-rays, gamma rays, and charged particles are types of radiation used for cancer treatment. The radiation may be delivered by a machine outside the body (external-beam radiation therapy), or it may come from radioactive material placed in the body near cancer cells (internal radiation therapy, also called brachytherapy). Systemic radiation therapy uses radioactive substances, such as radioactive iodine, that travel in the blood to kill cancer cells.
Radiation therapy kills cancer cells by damaging their DNA (the molecules inside cells that carry genetic information and pass it from one generation to the next) (1). Radiation therapy can either damage DNA directly or create charged particles (free radicals) within the cells that can in turn damage the DNA. Cancer cells whose DNA is damaged beyond repair stop dividing or die. When the damaged cells die, they are broken down and eliminated by the body’s natural processes. About half of all cancer patients receive some type of radiation therapy sometime during the course of their treatment.
Conventional Radiotherapy
Conventional external beam radiation therapy is the most common form of radiation treatment for Skull Base tumors. The goal of radiation is to destroy or stop a tumor. Radiation success depends on several factors: the type of tumor being treated (some are more sensitive to radiation than others) and the size of the tumor (smaller tumors are usually more treatable than larger ones). Some tumors are so sensitive to radiation that radiation therapy may be the only necessary treatment. Radiation can be used after a biopsy, or following partial or complete removal of a skull base tumor. When a tumor is surgically removed, some microscopic tumor cells may remain. Radiation attempts to destroy these remaining cells. Radiation is also used to treat inoperable tumors and tumors that have spread to the brain from another part of the body (metastatic brain tumors). Radiation may also be used to prevent metastatic brain tumors from developing.
Radiosurgery

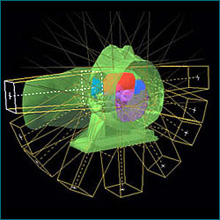
In radiosurgery, the word stereotactic hints at the three-dimensional coordinate system enabling co-identification of a virtual target on the patient’s diagnostic images in the treatment planning computer with the actual target position in the patient anatomy. Although technological improvements in imaging and computing, increased availability and clinical adoption have broadened the scope of radiosurgery in recent years, the localization accuracy and precision implicit in the word “stereotactic” remains of utmost importance for radiosurgical interventions today. Radiosurgery operates by directing tightly focused beams of ionizing radiation with high precision from multiple directions at intracranial and extracranial tumors and other lesions. The beam paths converge in the target volume, delivering a lethal cumulative dose of radiation, while exposing adjacent healthy tissue to a much smaller level of radiation.


